Professor Hamde Nazar sums up the event with PPIE member, Susan Mountain.
On 11th June 2025, the first of a series of events in June focussing on Virtual Wards (hospital at home) was hosted by the Newcastle NIHR PSRC. Representatives across many of the PSRCs contributed to the planning and organisation of this SafetyNet event.
Given the increasing drive for the use of technology in healthcare, the event brought together practitioners, researchers and patient and public representatives to discuss and consider the opportunity and challenges of the use of technology to support virtual ward service delivery.
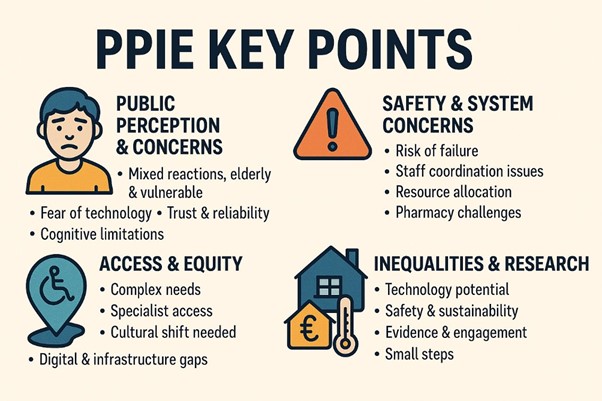
The day started off considering the patient and public voice first and foremost. The figure below summarises discussions from a patient and public involvement and engagement (PPIE) session held earlier in the year. Concerns were aired about the feasibility of technology being appropriate and accessible to all people, with other considerations voiced about the reliability of technology and trusting its effectiveness and security. People acknowledged that there are key challenges to address within the system around the workforce being properly resourced and trained, and about the existing IT infrastructure being fit for purpose. By the end of the discussion, people had ‘warmed’ to the idea, appreciating the opportunities for efficiency and potential improvements in care. However, people were keen to see small incremental developments with rigorous monitoring and evaluation to ensure people and patients were able to keep up and be reassured about the safety, equity and effectiveness of technological advancements within the NHS.
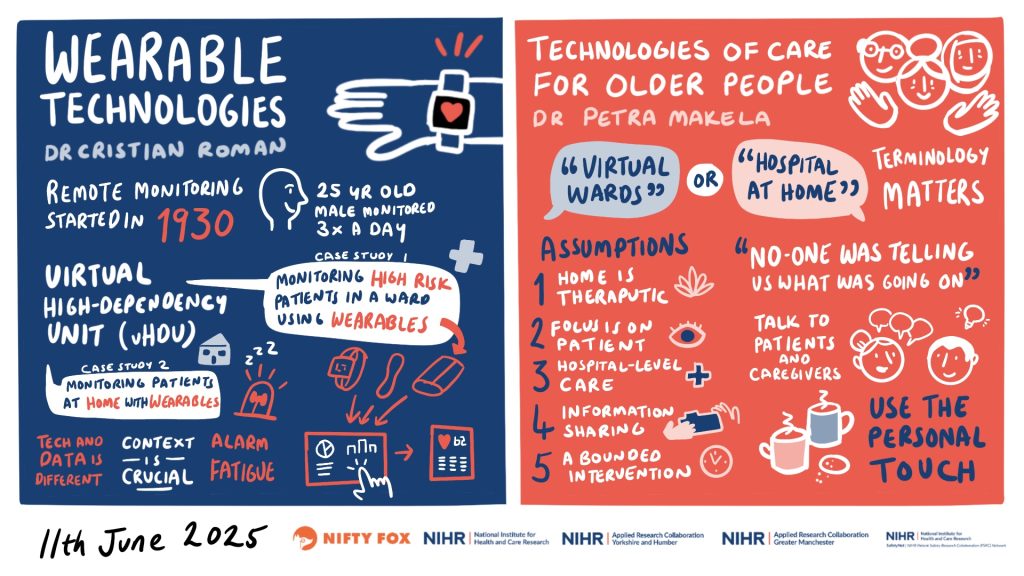
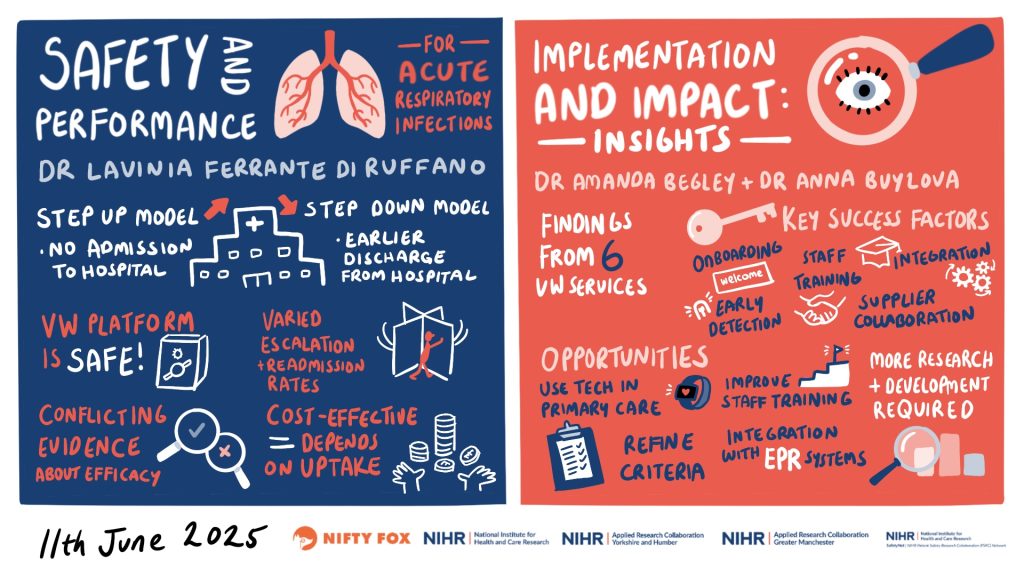
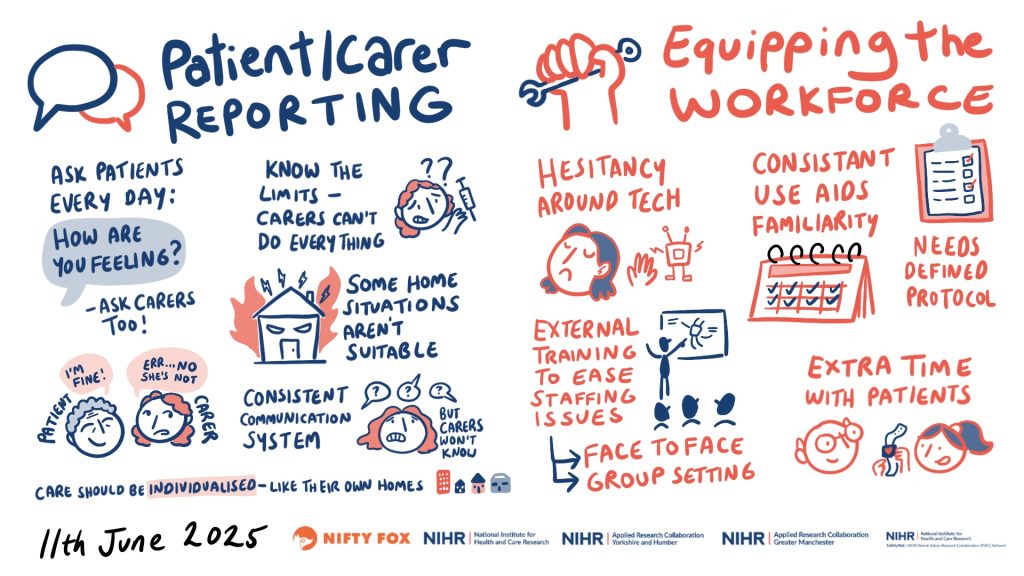
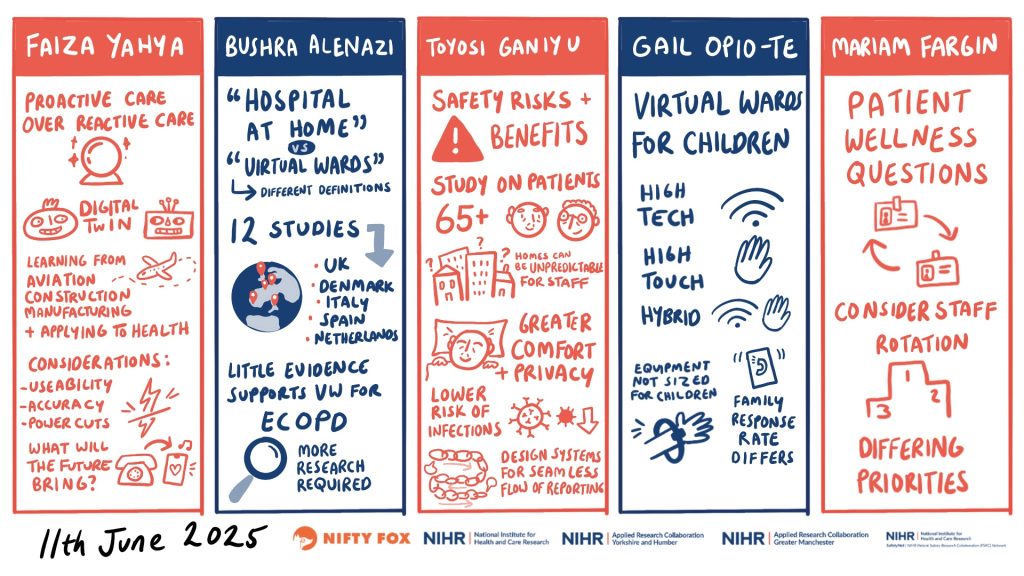
The event then included keynote speakers providing insight into existing evidence for the use of technology, with regards to effectiveness, impact on clinical outcomes and economic repercussions. These have been well captured in a series of scribes created by Claire Hubbard from Nifty Fox Creative.
The final panel discussion saw the keynote speakers tackling provoking questions posed by the audience, e.g., ‘how do we ensure equity in technology-enabled virtual wards?’, ‘what are the biggest challenges for the implementation of technology?’, ‘how sustainable is the use of technology in virtual wards?’
There was rich debate, and we can safely say we did not go away with all the answers. Virtual ward care, and technology use in this service model is a quagmire of half-knowns and unknowns. There is need for scrutiny and evaluation of service models to understand what is working, where, how and for which patients and their carers.
The recently released NHS 10-year plan frames technology as the default mechanism to engage with health by 2035. This means trying to understand how technology is deployed and used in virtual ward care is crucial and continued resource and engagement across practitioners, researchers and public and patient representatives is needed.

On that note, one of our patient and public representatives who attended the event provides her experience and takeaway thoughts:
My name is Susan Mountain and I live with multiple long-term conditions. I became involved with public involvement in 2019 and since then I have been part of many research projects, I am a public contributor to the PSRC, AI Multiply, ARC, CNTW, Sunderland University PCPI team, a campaigner for smoking cessation and I help with the Secure Data Environment.
I attended the SafetyNet Technology Enabled Virtual Wards event and found it very interesting. I heard many people talk of virtual wards but to be honest no one really convinced me that they are currently safe. I personally don’t think they are looking at the families that are involved when a patient is sent home using the virtual ward apparatus. I am concerned that there will be too much pressure on the family.
On that note, one of our patient and public representatives who attended the event provides her experience and takeaway thoughts:
I understand that there are benefits: it reduces the pressure on hospital beds; research has shown people recover quicker in home settings and it reduces the chances of infections in recovering patients.
They talked about patients being provided with medical devices to track vital signs and that all data would be transmitted to the hospital where it will be checked at regular intervals. It did worry me if the internet stops working, then how can they monitor. I had an elderly Mam in hospital and even in hospital I had to advocate for her so what would happen if she was at home?
I believe the PSRC has an important role to play in ensuring that this is fully researched before it is rolled out. It is also vital that staff are properly trained and that there is appropriate internet access in the cases selected for treatment at home.
By Prof Hamde Nazar, NIHR Newcastle PSRC

At the PSRC PhD SafetyNet event in March 2024, it became clear that were individual researchers and doctoral students investigating various safety aspects of a model of care known as virtual wards, currently gaining a lot of traction. Virtual wards, or hospital at home is not a new concept, but there has been increased drive to better manage patients in their home to avoid hospital admission and/or facilitate early discharge. Virtual wards allow patients of all ages to safely and conveniently receive acute care at their usual place of residence, including care homes.
After some corridor discussion, Prof Beth Fylan (Yorkshire and Humber PSRC) and Prof Hamde Nazar (Newcastle PSRC) decided to organise a collaborative Virtual Wards PSRC Safety Event.
In September, guest speakers, researchers, doctoral and pre-doctoral students across NIHR infrastructure were welcomed to the cross-PSRC Virtual Wards event in Newcastle University. The aim was to facilitate discussions to identify and develop research priorities and foster partnerships in this area of research.

The day was opened with an informative update by the virtual ward programme lead at NHS England, Charlotte Lynch. Charlotte provided an overview of the current evidence base and newly published Virtual Wards operational framework. It was recognised that there have been priority areas such as frailty, respiratory and heart failure and an increasing focus on children and young people. The national virtual wards team are keen to hear more evidence about what features of virtual wards are associated with positive outcomes and for which patients. There is interest to understand the longer-term impact on patients and establish how patient safety can be measured in this context.
Sophie McGlen then delivered interim findings on the barriers and enablers to implementation of virtual wards across the Midlands integrated care system. Sophie described the many factors across the system, organisation and practitioner levels that are important to consider around virtual ward implementation.
Maggie Westby provided an update on a realist review on virtual wards for patients with frailty. The key take home messages were around having more proactive care, keeping people safe and stable to prevent deterioration and potential crisis.
Representatives from four of the PSRCs (Newcastle, Yorkshire and Humber, Greater Manchester and North West London) showcased patient safety in virtual wards research projects.
Three round table discussions then focussed on:
- Research priorities for patient safety in virtual wards
- Potential methods and strategies to researching patient safety in virtual wards
- How to embed patient and public involvement and engagement and equality, diversity and inclusion into research
Attendees agreed on some key areas that required further evidence. namely:
- Establishing shared definitions and standards for virtual wards
- Investigating data availability, integration, sharing and governance for virtual wards
- Investigating patient safety in virtual wards – understanding appropriate metrics and strategies
- Investigating safe and appropriate patient assessment for and monitoring within virtual wards
- Understanding the need for and nature of workforce training, preparedness and competence
There was an appreciation that evaluations of virtual wards to date have been mainly single-site and observational in nature. There was a consensus that multi-site studies employing robust research designs, experimental where possible, are needed to improve the quality of the evidence base.
All attendees discussed the need for sustainable, well-resourced and diverse patient and public involvement to feed into all stages of the research process.

The final discussions of the day were to establish the next steps for this group given the shared interests and endeavours. There is an intention to set up a community of practice around patient safety in virtual wards where researchers can share, disseminate and signpost evidence and findings. The group are interested to explore the potential for collaboration for research and funding applications.
Researchers interested in joining the mailing list for the community of practice can contact Hamde Nazar from the Newcastle PSRC hamde.nazar@newcastle.ac.uk
Following on from this event, Prof Hamde Nazar has been invited to share the directions of research as identified by the PSRCs at a Virtual Wards sand pit event in October 2025 that is supported by the Advanced Care Research Centre based at the University of Edinburgh, the NIHR Applied Research Collaboration (ARC) North East and North Cumbria and Newcastle University.